Reclaiming Balance in Perimenopause
How Integrative Nurse Practitioners Solve the Problems That Conventional Care Misses
When a woman in her 40s walks into my exam room and says, “I feel like I’m falling apart,” she’s not just describing symptoms - she is describing a system in distress.
Perimenopause, mood swings, fatigue, and hormone chaos don’t ‘fit neatly’ into the 10-minute appointments or single-diagnosis protocols that prevail in traditional healthcare systems. These are multilayered problems, and solving them requires a whole-person, systems-aware approach that bridges body, mind, environment, and meaning.
This is where integrative nurse practitioners step in — and shine.
Who Am I as an Integrative Nurse Practitioner?
My name is Lindsay Fuson, PMHNP-BC, and I have been a nurse practitioner working primarily in the mental health care field and with women’s hormonal issues for over 8 years.
As a nurse practitioner, I am:
A licensed clinician with prescriptive authority and diagnostic training
Grounded in evidence-based medicine
Certified to manage both physical and mental health conditions
But as an integrative nurse practitioner, I am all of the above, but I go deeper. I am:
A systems thinker who understands the root causes behind symptoms
A translator of lab data + lived experience
A partner in healing who values patient story, not just patient chart
A clinician trained in nutrition, circadian medicine, psychoneuroendocrinology, and mind-body connection
A guide who sees you, not your labs
Now let me show you what that looks like in practice, through Maria’s story.
Meet Maria: A Woman at the Edge
Maria, 46, came to me feeling unlike herself. Her symptoms weren’t subtle:
Fatigue so intense she skipped social plans
Mood swings that left her snappy and then ashamed
Brain fog affecting her work as a teacher
Nighttime hot flashes and broken sleep
Irregular periods, low libido, and weight gain
A lingering sense of disconnection from her body, family, and purpose
She’d already been told “you’re fine” by her PCP — her basic labs were “normal.” She’d tried yoga and cut caffeine, but nothing helped.
Maria didn’t need reassurance. She needed root-cause care, personalized guidance, and someone who could see the whole picture.
That’s what I do.
How I Solved Maria’s Problem (And How I Solve Yours)
I didn’t start with a diagnosis. I started with a map — a framework I use in every patient: the Russian Doll Model of Integrative Care. It's how I assess the layers of your health, from your genes to your meaning.
Let’s walk through how I helped Maria, layer by layer.
-
Maria's symptoms pointed to metabolic drag: low vitamin D, sluggish thyroid, poor ferritin, and likely methylation challenges. I ordered a comprehensive panel (including hormone phase-specific testing), not just standard labs.
What I did:
Corrected her vitamin D (18 → 45 ng/mL in 8 weeks)
Supported thyroid conversion (selenium + adaptogens, no meds)
Boosted ferritin (28 → 65 with gentle iron + vitamin C)
Why I could do this: As an NP, I can interpret labs in context, order functional labs when needed, and prescribe what works — from nutrients to thyroid meds if required.
-
Her hormone testing revealed low progesterone in the luteal phase and rapidly fluctuating estradiol. Classic perimenopause.
What I did:
Introduced Vitex (chaste tree berry) for gentle progesterone support
Supported detox pathways (liver, gut) to help with estrogen clearance
Used magnesium glycinate for mood, sleep, and cramps
Balanced protein and fat at meals to stabilize blood sugar (and thus mood)
Why only I could do this: Unlike conventional care, I understand how hormones, nutrients, and neurotransmitters interact — and I don’t default to antidepressants unless needed. I restore your system instead of suppressing symptoms.
-
Maria scored 14 on a PHQ-9, showing moderate depressive symptoms. But what she was really experiencing was neuroinflammation + hormonal flux + meaning collapse.
What I did:
Referred her to CBT-I (insomnia-focused therapy)
Introduced her to journaling and reflection prompts: “What am I being asked to let go of?”
Guided her toward a values-aligned decision: reducing work hours by 1 class/week
Why this matters: I don’t just treat mood with pills. I help you decode your symptoms as messages. I treat root causes and empower you to take back control.
-
Maria’s bedtime was inconsistent, she skipped meals, and was glued to her phone until midnight. Her rhythms were off — which made everything worse.
What I did:
Created a circadian routine: morning sunlight, breakfast within 90 min, screen curfew
Recommended a short walk + magnesium bath nightly
Helped her track energy in relation to menstrual phases
Why only I do this: I am trained in chronobiology, behavior change, and personalized rhythm medicine. I don’t just say “get more sleep” — I coach you into it.
-
Maria was carrying everything: kids, career, and aging parents. No room to breathe.
What I did:
Helped her map her “invisible labor”
Gave her language to ask for more support from her partner
Connected her with a women’s perimenopause group for peer support
Why this matters: As an NP, my training is relational. I understand how burnout and biology intertwine — and I bring practical solutions grounded in compassion.
-
Maria’s final — and deepest — concern: “I’ve lost myself.”
What I did:
Helped her name this as a midlife metamorphosis, not a breakdown
Gave her reflective prompts:
“What parts of me are ready to rest?”
“What brings quiet joy?”
Encouraged her to restart painting — a passion from her 20s
This is what no lab can diagnose — but what I’m trained to witness, honor, and support.
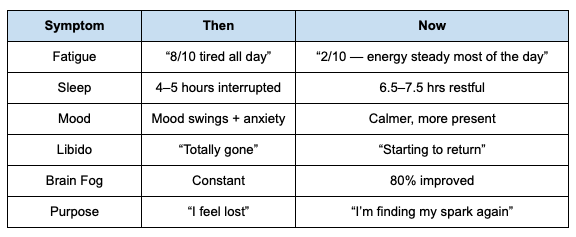
Three Months Later: Where Maria Stands Now
This Is What I Do — And Why It Matters
I don’t give you generic handouts or tell you “everything’s normal.”
I don’t medicate your spirit, blame your body, or ignore your story.
I do guide, test, teach, and hold space.
I do help women like Maria (and maybe like you) make sense of their symptoms, find their rhythm, and reclaim their vitality.
This is integrative nurse practitioner care.
And this is what only I, and colleagues trained in this model, can offer.
Is This You?
If you're feeling off in your 40s…
If your labs are “fine,” but you’re not…
If you’ve lost connection with your body, sleep, focus, or joy…
You’re not broken. You’re at a crossroads — and you deserve a map.
Want to work together?
Let’s build your personalized roadmap for mood, energy, hormones, and whole-self healing.
Contact my office or complete my patient screening form to schedule a 90-minute integrative consultation.*
We’ll uncover the root causes, run the right labs, and start a plan designed for your life, not just your labs.
*I also offer abbreviated 60-minute intakes depending on the complexity of symptoms, as well as a complimentary 15-minute introduction call if you want to learn more before scheduling a consultation.